Our Solution
Let's change the way the world sees and treats mental health.
Identifying the link between physiologic measures and mental health
Today, mental health assessments rely solely on patients reporting their symptoms which are by nature, subjective. Such subjectivity often impacts symptom reporting and therefore incorrect diagnosis and treatment.
Medibio’s technology will aid clinicians in the early detection of mental health conditions and empower individuals to screen and better understand their mental health.
MEB001
Medibio’s technology focuses on screening for depressive symptoms – known as a depressive burden.
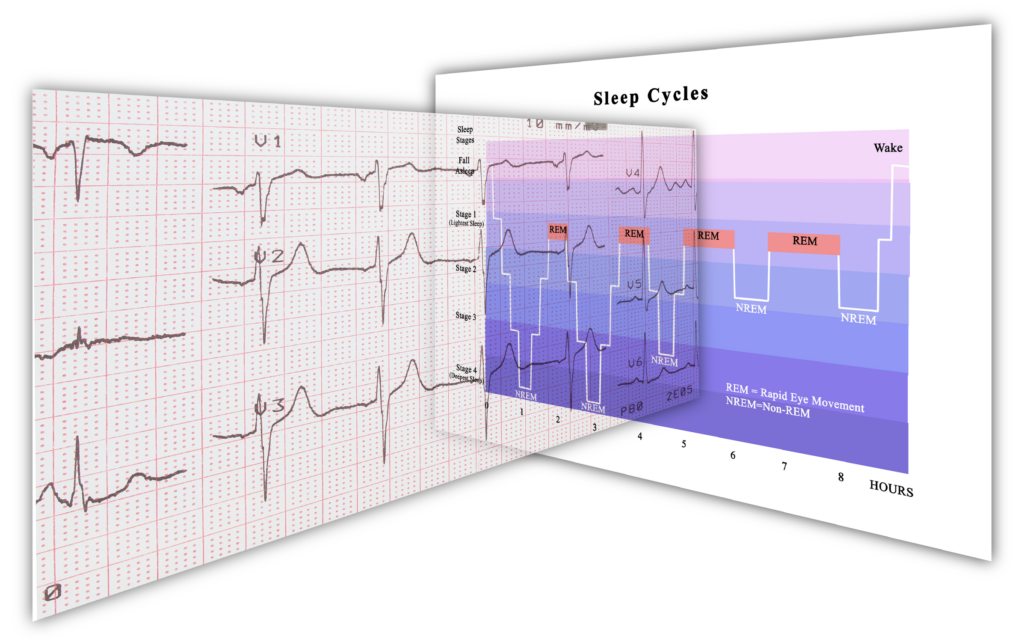
Data obtained from electroencephalographic (EEG) and electrocardiogram (ECG) recordings are processed through our proprietary algorithms in; sleep, nocturnal heart rate, and heart rate variability (HRV). The structural components of Medibio’s algorithms are developed based on Artificial Intelligence (AI). The algorithm development, build, and testing are supported by clinical pre-validation trials. These trials are followed by validation-to-commercialization trials performed with the highest FDA standards and according to the Agency regulations. Each clinical step of our validation process is consulted and presented to the FDA regulatory body for final approval.
HEART RATE VARIABILITY IS CRITICAL TO PHYSICAL, MENTAL & SLEEP HEALTH
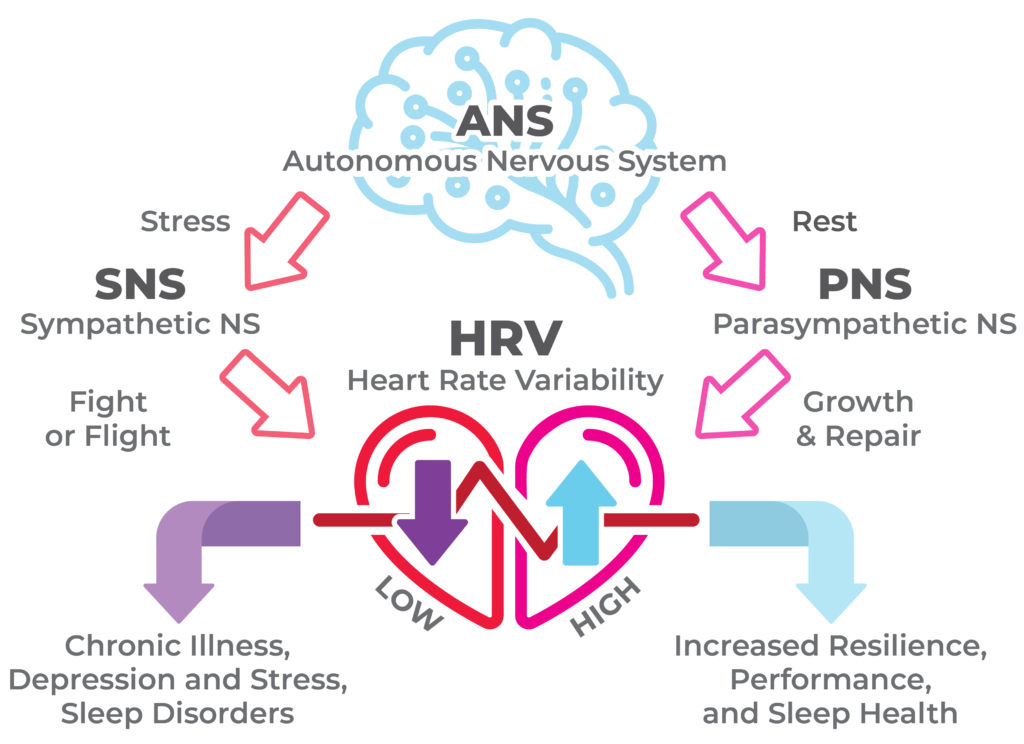
The determination of depressive burden is achieved by combining objective biomarkers of sleep macro and microstructures to heart rate and heart rate variability, to map autonomic modulation throughout sleep staging. The autonomic modulation is one of Medibio’s proprietary and novel technological features.
THE HRV CONNECTION